Insurance Reimbursement For Covid Testing
3182020 On June 23 2020 CMS issued FAQs on the Families First Coronavirus Response Act the Coronavirus Aid Relief and Economic Security CARES Act and other health coverage issues related to COVID-19 Part 43. Under the COVID-19 Claims Reimbursement to Health Care Providers and Facilities for Testing Treatment and Vaccine Administration for the Uninsured Program Uninsured Program health centers are eligible to seek reimbursement for conducting COVID-19 testing providing treatment for uninsured individuals with a COVID-19 diagnosis or for administering a licensed or authorized COVID.
 Ucla Ashe Center Covid 19 Testing
Ucla Ashe Center Covid 19 Testing
Laboratories using the test developed by the Center for Disease Control and Prevention CDC would be reimbursed 36 per test.

Insurance reimbursement for covid testing. 1 day ago These and other factors impact your reimbursement as the volume of tests has risen dramatically with the addition of serology tests to the COVID-19 diagnostic service mix. 6192020 Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a doctor. It turns out insurance companies are billed at a much higher rate than.
11302020 COVID testing is free for most of us but not for your insurance company. The FAQs were prepared jointly by the Department of Labor DOL the Department of Health and Human Services HHS and the Department of the Treasury. The projected value of these no-cost services will save members 97 million.
232021 Burned by Low Reimbursements Some Doctors Stop Testing for Covid Some insurers pay pediatricians less than the cost of the test itself jeopardizing a tool to help control the pandemic. After the tests are complete and results reported your labs next step is to create and code the claims. UnitedHealthcare will reimburse out-of-network providers for COVID-19 testing-related visits and COVID-19 related treatment or services according to the rates outlined in the Medicaid Fee Schedule.
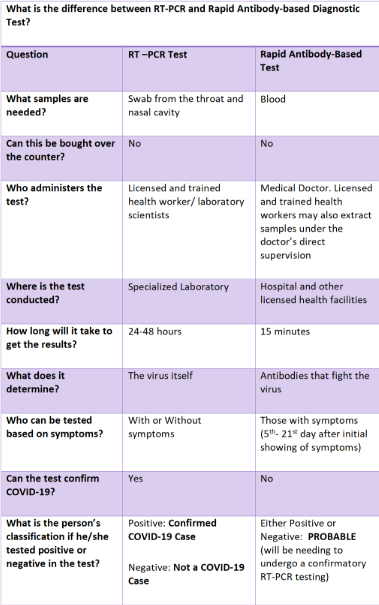
7132020 The FFCRA specifies that all COVID-19 testing approved by the Food and Drug Administration FDA or for which emergency use authorization EUA has been requested until the EUA has been ruled on. 3132021 Trip Interruption coverage. The CARES Act expanded the types of approved tests that were covered by the FFCRA and set the reimbursement rate for COVID-19 testing by out-of-network laboratories.
19 hours ago DoorDash partnered with Vault Health and Everlywell to offer on-demand COVID-19 PCR test kits. Health plans are required to cover most COVID-19 testing without cost-sharingsuch as deductibles co-pays and co-insurancewhen testing is ordered. This coverage will reimburse you for missed portions of your trip if youre forced into quarantine due to a positive Covid.
Health care providers who have conducted COVID-19 testing or provided treatment for uninsured individuals with a COVID-19 primary diagnosis on or after February 4 2020 can request claims reimbursement through the program electronically and will be reimbursed generally at Medicare rates subject to available funding. Under the CARES Act an insurer must reimburse an in-network laboratory at the negotiated rate that existed before the public health emergency and reimburse an out-of-network. 15 hours ago The test kit is available on DoorDash for 119 and may be eligible for reimbursement with healthcare insurance.
Private health insurance companies soon followed suit. 1 day ago COVID-19 testing and treatment cost share waivers and no-cost telehealth services will continue to be provided through June 30 to enable free access to physician-directed COVID-19 testing and treatment for commercially insured members. The Everlywell COVID-19 Test Home Collection Kit DTC uses a gentle lower nasal swab is FDA authorized for symptomatic and asymptomatic testing and does not require supervision.
11302020 The medicare reimburse rate for a nasal swab COVID test is a 100 dollars but theres no law that caps what a private facility can charge an insurance company. Is available on DoorDash for 119 and may be eligible for reimbursement with healthcare insurance. 9242020 The answer depends on who orders the test.
On March 16 the CMS released details about how COVID-19 testing would be reimbursed to health care providers administering the tests.
 The Laws Governing Covid 19 Test Payment And How To Improve Them
The Laws Governing Covid 19 Test Payment And How To Improve Them
 Covid 19 Testing And The Revenue Cycle Medical Laboratory Observer
Covid 19 Testing And The Revenue Cycle Medical Laboratory Observer
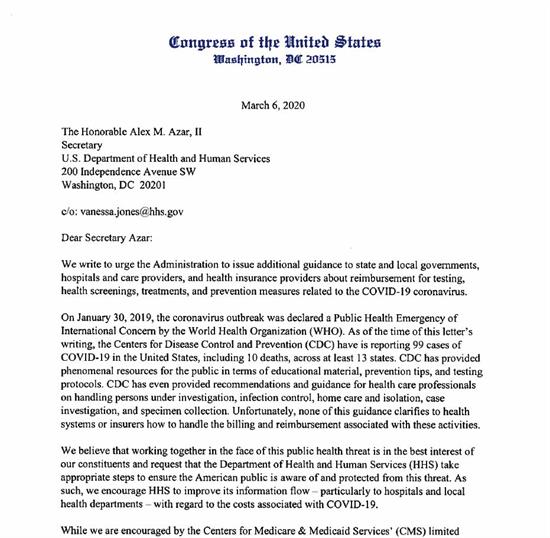 Balderson To Azar Guidance To State Local Governments Hospitals Needed On Reimbursements For Covid 19 Prevention Care U S Congressman Troy Balderson
Balderson To Azar Guidance To State Local Governments Hospitals Needed On Reimbursements For Covid 19 Prevention Care U S Congressman Troy Balderson
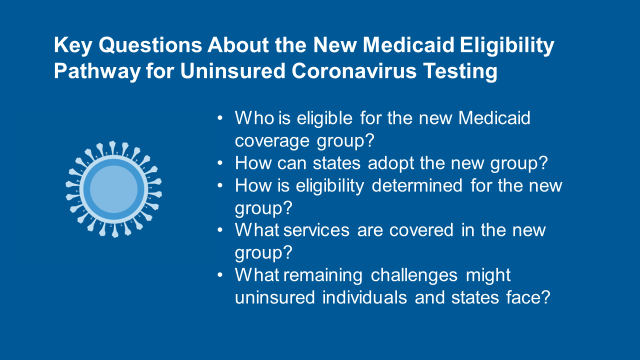 Key Questions About The New Medicaid Eligibility Pathway For Uninsured Coronavirus Testing Kff
Key Questions About The New Medicaid Eligibility Pathway For Uninsured Coronavirus Testing Kff
![]() National Health Insurance Administration Ministry Of Health And Welfare Taiwan Can Help National Health Insurance S Contribution In Combating Covid 19
National Health Insurance Administration Ministry Of Health And Welfare Taiwan Can Help National Health Insurance S Contribution In Combating Covid 19
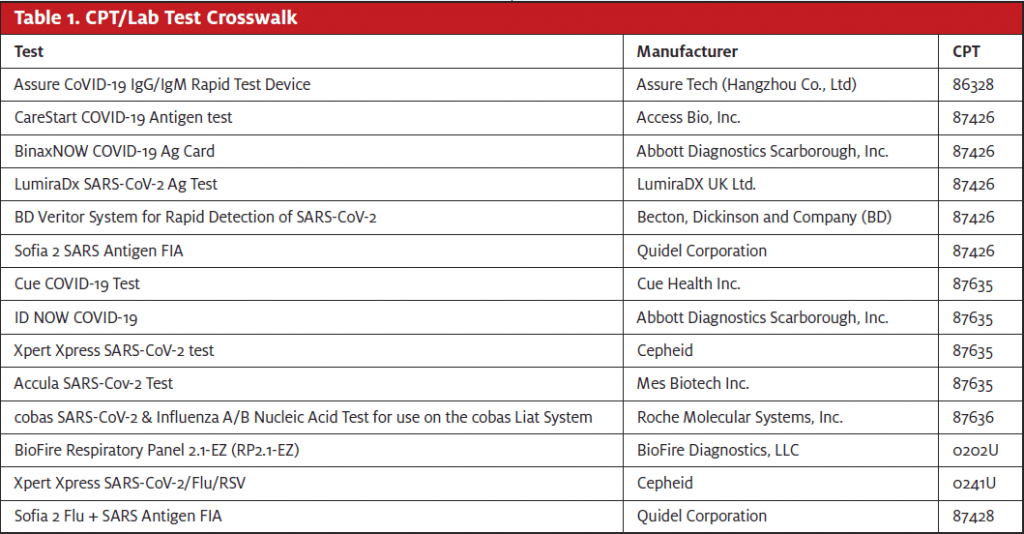 What S New For Rcm Updates On Coding For Covid 19 Testing Journal Of Urgent Care Medicine
What S New For Rcm Updates On Coding For Covid 19 Testing Journal Of Urgent Care Medicine
 Covid 19 Testing And The Revenue Cycle Medical Laboratory Observer
Covid 19 Testing And The Revenue Cycle Medical Laboratory Observer
 Covid 19 Coverage Personal Insurance Great Eastern Malaysia
Covid 19 Coverage Personal Insurance Great Eastern Malaysia
 How To File A Health Insurance Claim For Covid 19
How To File A Health Insurance Claim For Covid 19
 Philhealth Updates Grant Thornton
Philhealth Updates Grant Thornton
 Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
 Health Plans Banned From Denying Coverage Of Covid 19 Tests For Asymptomatic Individuals Healthcare Finance News
Health Plans Banned From Denying Coverage Of Covid 19 Tests For Asymptomatic Individuals Healthcare Finance News
 For Covid Tests The Question Of Who Pays Comes Down To Interpretation Kaiser Health News
For Covid Tests The Question Of Who Pays Comes Down To Interpretation Kaiser Health News
 Private Health Coverage Of Covid 19 Key Facts And Issues Kff
Private Health Coverage Of Covid 19 Key Facts And Issues Kff
 Covid 19 Archives Accountable Health Partners
Covid 19 Archives Accountable Health Partners


Post a Comment for "Insurance Reimbursement For Covid Testing"